PTSD and Addiction Treatment in Idaho
Stress and trauma are two of the most damaging and transformative influences a human being can ever experience. According to a 2022 report from the American Psychological Association (APA), at least 76% of adults in the United States admit they have experienced health issues that were as a result of unregulated stress.
While trauma ranks slightly lower than stress in the affected number of people, it is able to cause greater emotional and psychological damage. This is why many see a direct link between PTSD and addiction, as many people may turn to substances to treat the symptoms and negative emotions associated with PTSD. For successful and lasting treatment, it is often required that individuals work to heal their mental health. PTSD and substance abuse often go hand in hand, and true healing begins when the cycle of self-medication can be broken.

Before addressing PTSD and substance use, it’s important to know the underlying factors that can lead to both of them. Stress is a physiological and psychological response to dealing with pressure that exceeds an individual’s ability to cope (or at least their perceived ability). This can manifest as feelings of discomfort, tension, or anxiety.
Stress can result from a variety of factors, ranging from a person’s daily workload to prolonged substance abuse. Chronic stress can have adverse effects on mental and physical health, as well as overall quality of life. Many people turn to substances to work through stress, and co-occurring mental illnesses may also feel alleviated through this substance use.
What is Trauma?
Trauma refers to an emotional and/or psychological response to an event (or series of events) that are deeply distressing or disturbing. These experiences may overwhelm an individual’s ability to cope in the moment, which can lead to feelings of helplessness, fear, or powerlessness.
While fewer people deal with trauma than stress, it is believed to cause greater emotional and psychological damage. This is why many see a direct link between PTSD and addiction to substances, as many people who suffer from substance use disorders are also seeking trauma therapy to address underlying PTSD.
How are Trauma and Stress Connected?

While people might not experience daily events that are significant enough to be called traumatic, they may be exposed to a good deal of stress during the day. In many cases, the stress could be too much to process or handle, so people turn to drug abuse to cope with pent-up stress. Many people enter treatment for drug addiction without realizing that they also need to focus on reducing PTSD symptoms.
Types of Stress Disorders
Like the myriad differences one mind could have compared to others, people perceive and react to stress differently. If someone has access to support where they can discuss trauma-related symptoms, they may have a better ability to confront their trauma history. If they’re seeking treatment for addiction, such as during inpatient substance abuse treatment, they may feel more safe expressing uncomfortable feelings to the mental health professionals around them.
Regardless of the different nuances that stress may have on different people, there are generally five types of stress disorders:
- Generalized Anxiety Disorder (GAD)
- Panic Disorder
- Social Anxiety Disorder (SAD)
- Post-Traumatic Stress Disorder (PTSD)
- Obsessive-Compulsive Disorder (OCD)
Not all stress can manifest into a PTSD diagnosis. But it is important to know the symptoms of developing PTSD, so that treatment can be considered before drug addiction (or other unhealthy coping skills) make trauma processing even more difficult.
PTSD Symptoms That Can Overlap With Substance Abuse
Addiction and trauma often become a vicious cycle, as someone seeking safety from PTSD symptoms will turn to a substance that will only exacerbate their pain. This is why trauma and disorders associated with trauma can be risk factors for substance use disorder.
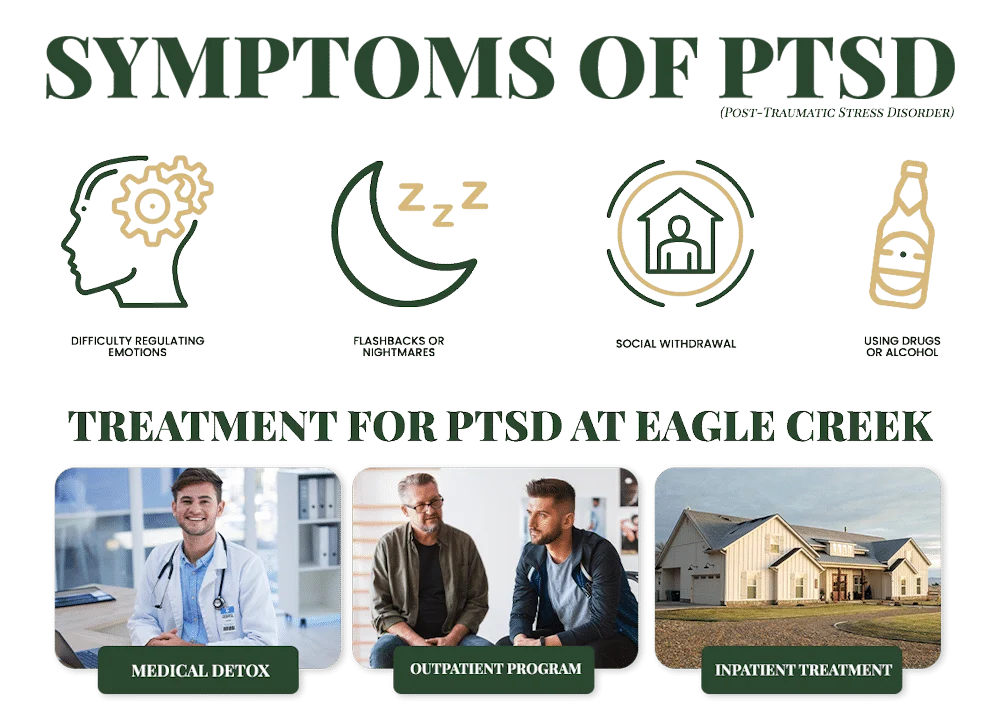
Someone suffering from addiction disorder and comorbid PTSD may show the following symptoms:
- Flashbacks or nightmares related to traumatic events, leading to increased substance use as a coping mechanism
- Using drugs or alcohol to numb emotional pain, alleviate anxiety, or escape intrusive memories
- Difficulty regulating emotions, such as heightened irritability mood swings, exacerbated by substance use
- Engaging in risky behaviors while under the influence, potentially re-traumatizing oneself or worsening existing trauma
- Social withdrawal, showing avoidance symptoms regarding triggering situations or people
- Physical health issues such as memory loss, further complicating recovery from trauma
- Challenges in seeking help or adhering to treatment for either addiction or trauma
In the US, an estimated 34.4% or people with post-traumatic stress disorder also suffer from a substance use disorder. These individuals were most likely to experience alcohol abuse disorders. It’s important to understand the similarities between drug abuse and PTSD symptoms, then respond accordingly to help people who experience traumatic events. Finding the right residential programs Idaho can make all the difference in providing structured care and support to heal from PTSD.
Contact Eagle Creek Ranch Recovery
Today!
Why Wait? Find The Help You Need By Reaching Out To Us Today! Our Admissions Team Is Standing By.
The Relationship Between Post-Traumatic Stress Disorder (PTSD) and Substance Abuse
Many people are not even aware that their trauma made them heavily dependent on alcohol or drugs, and thus don’t address the disorder at the heart of their addiction. Using substances to cope with PTSD is a common coping skill, but people who take this approach suffer poorer treatment outcomes for treating addiction and psychiatric disorders.
Sometimes, the treatment options for Post-Traumatic Stress Disorder itself can provoke a substance use disorder through pure chance. If someone is injured in the course of a traumatic event, such as in a car accident, they may develop a dependence on opioids (or other substances) that they use to mitigate the ordeal they suffer.

How Do PTSD and Substance Use Co-Occur?
The kind of trauma that military veterans suffered left most of them in a state of persistent paranoia, anxiety, fear, and even depression. Combined with the difficulty in readjusting to a peaceful life after active duty, many veterans turn to substance use. They may also wish to remain in a state where their minds won’t continually focus on the horror and violence they saw in combat. This is what often results in a dual diagnosis of PTSD and addiction. There are many support groups and resources for those with PTSD who abuse alcohol or drugs. but this was not always the case.
Who Suffers from PTSD and Substance Abuse?
Trauma that pushes people into addiction is not limited to people from the armed forces. Many victims of domestic abuse or physical assault develop an alcohol use disorder to avoid PTSD symptoms or confronting their history. But post-traumatic stress disorders and substance use disorders don’t go away on their own. Without individual therapy (and concurrent treatment), a person can suffer from both conditions for a prolonged period with no knowledge of what to do with their painful memories.
Treatments for PTSD and Substance Abuse
As part of dual diagnosis treatment for both PTSD and addiction, a mental health professional may also use prolonged exposure therapy or imaginal exposure techniques to help the person come to terms with their trauma history. But treating PTSD is highly dependent on the person themselves, their treatment options, and the circumstances that lead them to pursue a PTSD diagnosis.
If a person suffers from other mental disorders, such as a stress disorder, those need to be taken into account when designing PTSD and/or substance dependence treatment plans. This may also influence decisions to do certain treatments like exposure therapy. It’s necessary to have a dual diagnosis perspective when treating substance use disorder that may have at least partly resulted from PTSD symptoms.
Cognitive-Behavioral Therapy (CBT)

For those who do receive treatment, one of the most effective approaches used by therapists to help people with co-occurring PTSD and addiction is cognitive behavioral therapy. This modality of therapy features techniques that allow the person to isolate and address the troublesome thoughts and behavioral patterns that feed their need to indulge in substance abuse.
CBT seeks to help the person arrive at a correct response when confronted by the emotional and psychological stress brought on by PTSD. This starts by removing the option of alcohol or drugs as a response to the problem. From there, the focus then moves to relapse prevention and overall addiction treatment. Sometimes medication will be used to ease addiction or withdrawal symptoms. But this is highly dependent on the individual, their traumatic event, the presence of a mental illness, whether they have other substance use disorders, if they have a stress disorder, and their needs for addiction treatment.
Find Healing at Eagle Creek Ranch Recovery for PTSD and Substance Abuse
At Eagle Creek Ranch Recovery, where we deal with the issue of trauma and co-occurring substance abuse the way it should be dealt with: from the inside out. With evidence-based approaches, careful assessment, and a good deal of support, you’ll be on the road to recovery. Contact us today to get started.


Clinical Director
Kendall Maloof is the clinical director at Eagle Creek Ranch Recovery. She is a licensed marriage and family therapist and has held multiple leadership roles before settling here at Eagle Creek Ranch Recovery. Kendall received her master’s degree in marriage and family therapy from the Chicago School of Professional Psychology in 2016. Her career in mental and behavioral health began in 2014 when she took up internships in both the nonprofit and for profit sectors. She interned at multiple reputable companies, such as The Living Success Center and 449 Recovery in California.
In 2019, Kendall became the clinical director of Sunsets Recovery for Woman, a dual diagnosis program in southern California. Kendall is a natural leader. She has an incredible ability to problem solve and stay calm in any situation. Kendall never fails to show up when she is needed, and her calm demeanor makes her team and clients feel at ease. Eagle Creek Ranch Recovery is proud to have Kendall as our clinical director.


