Over time, people have come to associate different mental illnesses as being connected to certain groups of people. While certain groups of people may be diagnosed with certain mental illnesses more frequently, there are no inherent limitations on who can have a certain mental illness. Depression-based disorders in particular do not discriminate.
However, men have historically been alienated from treatment and discussion about depression care. It was sometimes considered a weakness for a man to show any signs of having depression. Men were frequently told to “toughen up” or “don’t be a sissy” when opening up about feeling sad. Thankfully, this is no longer the standard approach to mental health treatment in most societies. But many men still feel unable or unwilling to seek help for depression. They may not even recognize it in themselves, so it’s important to know and spot the signs.
General Causes of Depression
Common causes of depression include a complex interplay of genetic, biological, environmental, and psychological factors. It can be triggered by a cause, or be an underlying state in the form of clinical depression.
Common triggers for depression include:
Family history and genetic disposition plays a role in developing depression, with individuals with a family history of depression being at a notably higher risk.
If individuals are undergoing medical treatments or taking medications that affect levels of serotonin, dopamine, and norepinephrine, they have an increased chance of developing depression.
Outside factors in a person’s life, such as trauma, loss, financial difficulties, or relationship problems, can trigger or exacerbate the development of depression.
Treatment for certain illnesses, including substance abuse, can increase the risk of depression. This is why it’s important to seek dual diagnosis treatment when entering rehabilitation for addiction.
People who naturally have a higher rate of pessimism or low self-esteem may be more at risk of developing depression.
As people age, their ratios of certain hormones change. This is natural, but these changes on top of treatments for aging or developing health problems may increase the risk of developing depression.
It should be noted that not everyone will experience depression when faced with difficult life circumstances, and it doesn’t mean that those who do are weak in any way. Those with a family history of depression or similar mental illness will be more inclined to respond in that way. It may also be a reaction to different events coming
Specific Signs of Depression in Men
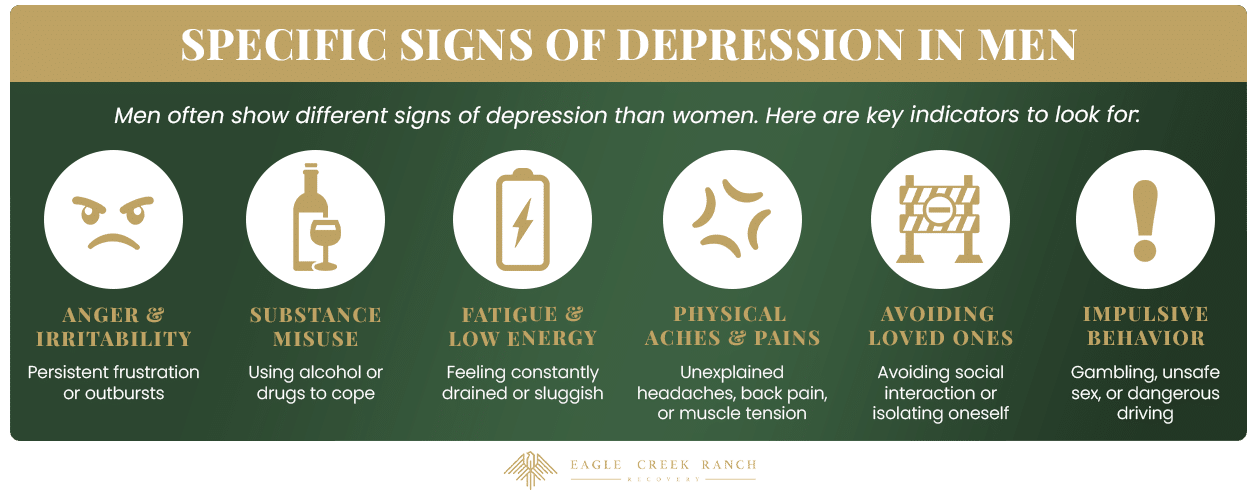
Symptoms that may emerge more prominently in men include:
- Increased irritability or anger
- Physical complaints, such as headaches, digestive issues, or chronic pain
- Risk-taking behavior or escapism
- Increased working hours
- Difficulty expressing emotions
- Loss of interest in previously enjoyed activities
Recognizing these gender-specific signs can help in early identification and treatment of depression in men.
How Is Depression Different For Men Than Other Genders?
Men may experience barriers to seeking help for depression, largely due to societal norms around masculinity and mental health stigma. However, this can take many forms:
- Traditional Gender Roles: Men may feel pressure to conform to traditional gender roles, which often emphasize stoicism, self-reliance, and emotional restraint.
- Fear of Judgement: A man suffering from depression may be more reluctant to acknowledge their feelings or seek professional help, fearing judgment or appearing weak to others.
- Being Unsure of Where to Turn: Men may also be less likely to discuss their mental health concerns with friends or family members, further delaying or preventing them from accessing treatment.
- Unhealthy Coping Techniques: Men may cope with depression through avoidance, substance use, or other unhealthy coping mechanisms. They may copy coping mechanisms they saw used by other men while growing up, in a time before seeking help for mental illness was considered socially acceptable for men.
The Men’s Mental Health Crisis
Because of previous stigma and a lack of awareness around men’s mental health, there has been an incredible spike in mental health problems for men in America. As of 2018, men are up to seven times more likely than women to commit suicide. About 84% of all men who committed suicide during the surveyed period had no recorded history of mental illness, suggesting that the men did not receive ongoing care for mental illness. Suicide has been named as the sixth leading cause of death for men in America, and the rate of suicide was ranked as four times higher for men as for women in 2021.
The men’s mental health crisis encompasses a range of challenges, and there is no easy solution. Stigma surrounding mental illness can perpetuate a cycle of suffering in silence. Additionally, limited access to mental health resources and culturally insensitive approaches to care can hinder men’s treatment.
Common Co-Occurring Conditions For Men With Depression
Men with depression commonly experience co-occurring conditions that can exacerbate symptoms and complicate their treatment. These may include:
Men with depression often also experience anxiety disorders such as generalized anxiety disorder (GAD), social anxiety disorder, or panic disorder.
Depression and substance abuse frequently coexist, as some men may turn to alcohol or drugs as a way to cope with their depressive symptoms.
Depression can contribute to sexual dysfunction, including erectile dysfunction. This can impact a man’s self-esteem and further worsen depressive symptoms.
There is a negative relationship between depression and heart disease, with each condition increasing the risk of the other. But men with depression may have a higher prevalence of cardiovascular issues, and should inform their medical professional of their depression if they are predisposed to heart problems.
Depression and chronic pain can often co-occur, with each condition exacerbating the other. Men with depression may experience physical symptoms such as headaches, back pain, or gastrointestinal issues. This may also be a way depression can manifest in men if they are not inclined to openly showing emotions.
Ties Between Depression and Addiction
Depression and addiction often coexist in a complex relationship. Individuals with depression may turn to addictive substances as a way to self-medicate or cope with their emotional pain. Chronic substance abuse can lead to changes in brain chemistry and structure, increasing the risk of developing depression or worsening existing depressive symptoms.
The presence of both depression and addiction can complicate treatment and increase the risk of relapse. Addressing both conditions through dual diagnosis treatment is crucial for achieving long-term recovery and mental health stability.
How to Support Someone With Depression
It may be difficult to know how to support a man during a mental health crisis, especially if he is not typically communicative about his feelings. But men still need support, and there are a few ways to offer support during a difficult time:
- Listen Without Judgment: Provide a safe space for the men in your life to express their feelings and concerns without fear of criticism or judgment.
- Offer Validation: Acknowledge their emotions and let them know that you understand and appreciate them sharing their struggles. Offer empathy if the situation feels correct, but make sure not to make the situation about you.
- Encourage professional help: Support them in seeking professional treatment, and offer to help them find resources or accompany them to appointments if needed. If they need to take medication or perform other tasks as part of treatment, encourage them to follow through.
- Be Patient and Understanding: Understand that recovery from depression takes time and may involve setbacks and backsliding. Offer patience and encouragement, and do not expect them to be better overnight.
- Stay Connected: Keep in touch regularly, whether through online chats, text messages, or spending time together in person. It’s important to convey that they are not “untouchable” because they have depression.
- Encourage Self-Care: Encourage them to engage in activities they enjoy, as well as prioritize self-care practices like exercise, eating healthy food, and taking in adequate sleep.
- Respect Boundaries: Understand that a man with depression may need space to process emotions. Respect this need, and try to set ground rules so no one’s feelings are hurt.
Remember that supporting someone with depression can be challenging, and it’s important to also care for your own needs during this process. Your presence and care can make a significant difference. But it’s important to make sure you have enough emotional support to give.
Eagle Creek Can Support Healing From Depression in Recovery
Suffering from depression isn’t something anyone should face alone. At Eagle Creek Ranch Recovery, we work to support men battling mental illness, addiction, and the combination of the two. As a single-gender facility, we’re invested in speaking to men’s needs and giving them a safe space to express feelings and go through the process of healing. It’s never too late to ask for help. Contact us today, and learn just how much help is out there for someone suffering from depression.

Clinical Director
Kendall Maloof is the clinical director at Eagle Creek Ranch Recovery. She is a licensed marriage and family therapist and has held multiple leadership roles before settling here at Eagle Creek Ranch Recovery. Kendall received her master’s degree in marriage and family therapy from the Chicago School of Professional Psychology in 2016. Her career in mental and behavioral health began in 2014 when she took up internships in both the nonprofit and for profit sectors. She interned at multiple reputable companies, such as The Living Success Center and 449 Recovery in California.
In 2019, Kendall became the clinical director of Sunsets Recovery for Woman, a dual diagnosis program in southern California. Kendall is a natural leader. She has an incredible ability to problem solve and stay calm in any situation. Kendall never fails to show up when she is needed, and her calm demeanor makes her team and clients feel at ease. Eagle Creek Ranch Recovery is proud to have Kendall as our clinical director.





