Alcohol is an easily available substance that is recreationally used across the world. People include it as part of daily meals, nights out, and celebrations. But excessive alcohol intake can lead to alcohol dependence.
Most people do not realize that this widely-consumed substance can cause seriously uncomfortable symptoms that make it difficult to quit. Most people who drink alcohol don’t typically experience an extreme timeline of alcohol withdrawal. However, those who have used alcohol for an extended period of time may be at risk for serious symptoms that are not only uncomfortable but potentially dangerous.
Alcohol withdrawal symptoms are different for everyone, and everyone’s reactions are different as well. If you or someone you love is quitting drinking, there are some typical withdrawal symptoms you can expect during the timeline of alcohol withdrawal.

When Does Alcohol Withdrawal Begin?
Alcohol withdrawal syndrome (AWS) begins when someone suddenly stops drinking alcohol or seriously reduces their amount of consumption. AWS includes a group of symptoms that will begin to occur as the body processes the alcohol within the body with no (or very little) replacing what was previously there. AWS occurs in individuals who have been drinking heavily and consistently for an extended period of time.
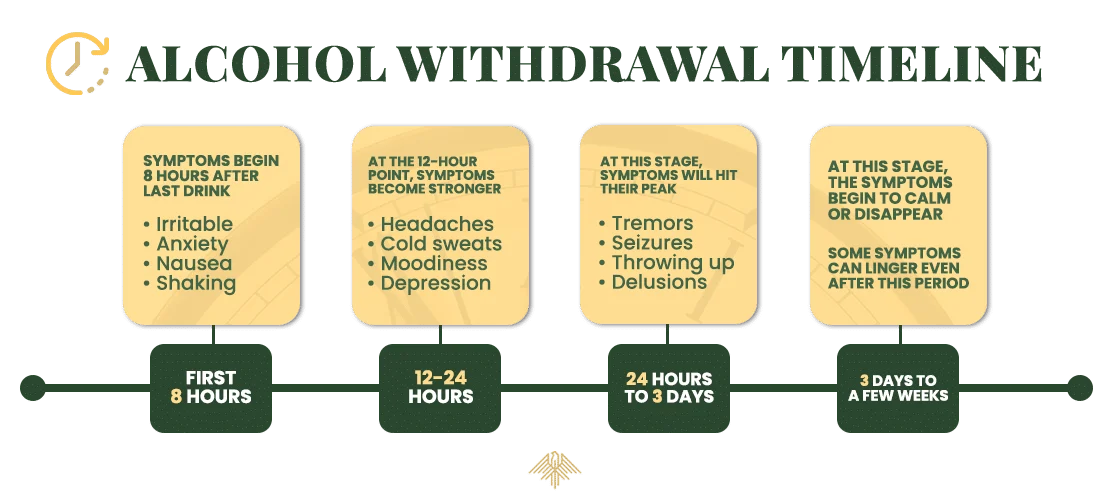
For people suffering from alcohol dependence, the symptoms of alcohol withdrawal will typically begin around the first eight hours after their last drink. In the early timeline of alcohol withdrawal, the symptoms are somewhat mild but begin to get progressively worse over time.
Symptoms may include:
- Irritability
- Anxiety
- Pale, sweaty skin
- Loss of appetite
- Nausea
- Shaking
After 12 hours of being without alcohol, people typically start to experience more pronounced symptoms of alcohol withdrawal. For individuals who were engaging in alcohol abuse in great amounts and at a great length of time, their symptoms will be much more noticeable and severe. At this point, an individual may experience:
- Headaches or migraines
- Cold sweats or sweating at night
- Cognitive decline (brain fog)
- Difficulty sleeping
- Moodiness
- Throwing up
- Depression
- Nightmares or vivid dreams
- Hallucinations
This is typically the worst part of the alcohol withdrawal timeline, as symptoms will peak in severity. The onset can be as early as 24 hours or three full days after the last drink. To prepare for this timeframe, individuals should expect to experience more uncomfortable symptoms and have resources available.
Symptoms can include:
- Throwing up
- Stomach discomfort
- Tremors
- Seizures
- Delusions
- Extreme agitation
- Delirium tremens (which require emergency medical attention)
For most individuals going through alcohol withdrawal, the symptoms should start to calm or disappear after three days. However, many factors can alter this timeline and it is important not to establish a hard and fast timeline. Other symptoms like depression, anxiety, and moodiness that can last for a few weeks (or even longer)..
What Factors Impact The Alcohol Withdrawal Timeline?
The alcohol withdrawal timeline can be influenced by several factors, including:
The duration of alcohol use plays a significant role in shaping the alcohol withdrawal experience and substance abuse treatment plans. For individuals with a short-term history of heavy alcohol use, withdrawal symptoms are generally milder and may include anxiety, mild tremors, and nausea. These symptoms typically resolve within a few days to a week, requiring less intensive support. Those who have engaged in long-term alcohol use may require medications like benzodiazepines to mitigate severe symptoms and prevent complications.
Heavy alcohol intake significantly impacts the intensity of alcohol withdrawal symptoms and the approach to treatment. Individuals who engage in heavy alcohol use are more likely to experience severe withdrawal symptoms, including intense tremors, hallucinations, seizures, and even delirium tremens. This is a serious condition characterized by confusion and autonomic nervous system instability. These symptoms necessitate close supervision, as medical complications (including death) can occur.
The frequency of drinking plays a crucial role in determining the complexity of the alcohol withdrawal process. Individuals who engage in regular, daily drinking are likely to encounter more challenging stages of alcohol withdrawal than those who binge drink occasionally. Those who drink alcohol regularly often develop a higher level of physical dependence, leading to more severe withdrawal symptoms such as intense cravings, anxiety, irritability, and possibly life-threatening conditions like alcohol withdrawal seizures or delirium tremens.
Individuals in good health may experience a more straightforward alcohol withdrawal process, while those with underlying health issues might face more severe alcohol withdrawal. Age is another critical factor, as older individuals may experience withdrawal symptoms more severely due to a slower metabolism and the presence of age-related health conditions. Pre-existing medical conditions such as liver disease, cardiovascular issues, or mental health disorders can exacerbate alcohol withdrawal symptoms, making the process more complex and potentially dangerous.
Some individuals may have a genetic makeup that makes them more sensitive to the effects of alcohol, leading to more intense alcohol withdrawal syndrome. Others might have genetic variants that impact the metabolism of alcohol, affecting how quickly withdrawal symptoms set in and how long they last.
Individuals who have undergone withdrawal before may encounter more intense symptoms in future attempts due to a phenomenon known as kindling. This occurs when the brain becomes more sensitized to the effects of alcohol withdrawal over time. This sensitization can lead to increased anxiety, more severe tremors, and a heightened risk of seizures during subsequent alcohol withdrawal episodes.
Concurrent substance abuse can significantly complicate alcohol withdrawal, presenting unique challenges that require immediate medical attention. When individuals use other substances alongside alcohol, it can intensify withdrawal symptoms and introduce additional health risks. For example, the combination of alcohol with depressants like benzodiazepines can enhance sedation and respiratory depression.
Psychological factors play a pivotal role in the severity and duration of alcohol withdrawal symptoms, profoundly influencing the treatment approach. Mental disorders such as anxiety and depression can exacerbate alcohol withdrawal symptoms, making the experience more challenging and prolonged. These emotional states not only intensify the physical symptoms of withdrawal but also increase the risk of relapse, as individuals may turn to alcohol as a means of self-medication.
What Happens to the Body and Brain During Alcohol Withdrawal?

During alcohol withdrawal, the body and brain undergo several changes as they adjust to the absence of alcohol. This can lead to a range of symptoms:
Body
- Autonomic Nervous System Activation: The sudden absence of alcohol, a depressant, leads to an overactive autonomic nervous system. This can cause symptoms like sweating, increased heart rate, and high blood pressure.
- Tremors and Shakes: Commonly known as “the shakes,” these are caused by the nervous system’s heightened state of activity.
- Gastrointestinal Distress: Nausea, vomiting, and diarrhea can occur as the digestive system reacts to the absence of alcohol.
- Sleep Disturbances: Insomnia and vivid dreams are common as the body struggles to regulate sleep patterns without alcohol.
Brain
- Neurotransmitter Imbalance: Alcohol affects neurotransmitters like GABA and glutamate. During withdrawal, the brain struggles to rebalance these chemicals, leading to symptoms like anxiety, irritability, and seizures.
- Cognitive and Mood Changes: Individuals may experience confusion, difficulty concentrating, anxiety, and symptoms of depression as the brain adjusts to functioning without alcohol.
- Risk of Seizures: Severe withdrawal can lead to seizures, due to the brain’s overactivity and neurotransmitter imbalance.
- Delirium Tremens (DTs): In severe cases, individuals may experience delirium tremens (DTs), characterized by severe confusion, hallucinations, and autonomic instability that can be life-threatening.
These symptoms highlight the importance of seeking help from medical professionals to safely manage alcohol withdrawal, especially for those who drink heavily or have experienced previous withdrawal episodes.
Is Quitting Drinking Suddenly Dangerous?
Most people who try to quit drinking alcohol cold turkey find that the timeline of alcohol withdrawal symptoms is extremely uncomfortable but not typically dangerous. But in severe cases of chronic alcohol use disorder, quitting drinking can be deadly. If you are unsure how serious your alcohol consumption may be, it’s best to speak to an addiction specialist to gain perspective.
How Can I Help Someone Going Through Alcohol Withdrawal?

The best thing you can do is get them to a reputable detox facility to help assist with overcoming alcohol withdrawal symptoms. Medical detox ensures they have the professional support they need if any complications arise. If detox is not an option and the individual has mild withdrawal symptoms, help keep the person comfortable and make sure their schedule is clear. You’ll also want to make sure that they have plenty of water and healthy foods on hand. Most importantly, make sure they do not have easy access to alcohol.
Contact Eagle Creek Ranch Recovery Today to Learn More About Alcohol Withdrawal Syndrome
If you or someone you love is struggling with alcohol use disorder, don’t wait to get help. Eagle Creek Ranch Recovery is located in beautiful Nampa, Idaho (close to Boise!) and offers a serene setting to work through alcohol withdrawal treatment and recover with dignity. Our treatment staff is fully invested in making sure you overcome alcohol abuse and develop the skills necessary to progress forward in recovery. Contact our team today to learn more.

Clinical Director
Kendall Maloof is the clinical director at Eagle Creek Ranch Recovery. She is a licensed marriage and family therapist and has held multiple leadership roles before settling here at Eagle Creek Ranch Recovery. Kendall received her master’s degree in marriage and family therapy from the Chicago School of Professional Psychology in 2016. Her career in mental and behavioral health began in 2014 when she took up internships in both the nonprofit and for profit sectors. She interned at multiple reputable companies, such as The Living Success Center and 449 Recovery in California.
In 2019, Kendall became the clinical director of Sunsets Recovery for Woman, a dual diagnosis program in southern California. Kendall is a natural leader. She has an incredible ability to problem solve and stay calm in any situation. Kendall never fails to show up when she is needed, and her calm demeanor makes her team and clients feel at ease. Eagle Creek Ranch Recovery is proud to have Kendall as our clinical director.



